Der Medizinischen Fakultät der Friedrich-Alexander ... · SYSTEMIC-TO-PULMONARY ARTERY SHUNTING...
Transcript of Der Medizinischen Fakultät der Friedrich-Alexander ... · SYSTEMIC-TO-PULMONARY ARTERY SHUNTING...

SYSTEMIC-TO-PULMONARY ARTERY SHUNTING USING HEPARIN- BONDED GRAFTS
(“Systemiko-pulmonale Shunts unter Verwendung von Grafts mit kovalent an der Oberfläche gebundenem Heparin“)
Der Medizinischen Fakultät
der Friedrich-Alexander-Universität
Erlangen-Nürnberg
zur
Erlangung des Doktorgrades Dr. med.
vorgelegt von
Ambarsari, Yuletta Adny
aus Bangil (Indonesia)

Als Dissertation genehmigt von der
Medizinischen Fakultät der Friedrich-Alexander-Universi tät
Erlangen-Nürnberg
Vorsitzender des Promotionsorgans: Prof. Dr. Dr. h.c. J. Schüttler
Gutachter: PD Dr. Andre Rüffer
Gutachter: Prof. Dr. Robert Cesnjevar Tag der mündlichen Prüfung: 05. Dezember 2017

TABLE OF CONTENTS
ABSTRACT (English Version)……………………………………………..……... 1
ABSTRACT (German Version)……………………………………………..…..... 3
1. INTRODUCTION………………………………………………………….. 5
1.1. Palliative Shunting: A Brief Surgical History……………………................ 5
1.2. Shunt Associated Problems and Possible Drawbacks……………................ 8
1.3. Experience with "Heparin-Bonded" Shunts………………………………... 9
1.4. Aim of the Study…………………………………………………………… 10
2. MATERIAL AND METHODS……………………………………………. 11
2.1. Patients……………………………………………………………............... 11
2.2. Surgical Technique………………………………….……………………… 11
2.3. Follow-up…………………………………………………………………... 12
2.4. Statistical Analysis……………………………………………………….… 13
3. RESULTS…………………………………………………………………... 14
3.1. Patient Characteristics and Operative Data………………………................ 14
3.2. Survival…………………………………….……………………………….. 16
3.3. Shunt Patency………………………………………………………….…… 19
4. DISCUSSION…………………………………………………………….… 23
4.1. Survival……………………………………………………………………... 23
4.2. Shunt Patency…………………………………………………………….… 24
4.3. HBPS……………………………………………………………………….. 24
4.4. Limitations……………………………………………………….……...….. 25
4.5. Conclusion…………………………………….……………………………. 25
5. REFERENCES………….………………………………………………….. 26
6. ABBREVIATIONS………………………………………………................ 31
7. LIST OF FIGURES…………………………………………………….…... 32
8. LIST OF TABLES……………….…………………………………………. 33
9. ACKNOWLEDGEMENTS…………..…………………………………….. 34
10. DISCLAIMER…………………………………………………………….... 35

1
ABSTRACT (English Version)
Objectives:
Systemic to pulmonary artery shunting remains an important palliative procedure in
the staged management of complex congenital heart defects. The use of Heparin-
bonded polytetrafluorethylen shunts (HBPS) should enhance graft patency. This
study aimed to review the single-center experience with HBPS in the context of
congenital cardiac surgery.
Methods:
The records of 52 patients treated with HBPS between 2010 and 2016 were
retrospectively reviewed. Median age and weight were 8 days (range 3 – 83 days)
and 3.2 kg (range 1.8 – 5.7 kg), respectively. Selected shunt size was 3.5 mm in all
except 1 patient (4.0 mm). Fourteen patients (26.9%) were planned for future
biventricular repair and 38 patients (73.1%) went the univentricular pathway. Shunt
modifications included central aorto-pulmonary shunts (n=35; 67.3%) and modified
Blalock-Taussig shunts (n=17; 32.7%). Shunt patency and survival until estimated
second procedure were calculated using the Kaplan-Meier method.
Results:
Shunt patency was 90 ± 4% after a median duration of 133 days (range: 0 - 315).
Early mortality (30 days) was 5.7% (n=3). Another 3 patients died during their
hospital stay. The cause of death was not shunt-related in all patients. Five patients
developed subtotal HBPS thrombosis, either intraoperatively (n=3), early
postoperatively after 3 days (n=1; 1.9%) or late after 41 days (n=1; 1.9%). Treatment
of those patients comprised RVOT-opening (n=2; 3.8%) or new shunting (n=3;
5.8%). Elective shunt take-down was performed during corrective surgery (n=10;
19.2%), bidirectional Glenn (n=25; 48.1%) or shunt replacement (n=5; 9.6%). At the
end of follow-up, 1 patient (1.9%) had still a HBPS in situ. The survival rate until
planned second procedure was 84 ± 6% in univentricular patients, and 100% in
biventricular patients (p=0.14), respectively.

2
Conclusions:
The use of HBPS in the context of palliative heart surgery is safe and seems to
warrants long-term patency of systemic-to-pulmonary shunts. However, by
influencing thrombosis on only one site of Virchow’s triad, shunt thrombosis,
occurring predominantly early, cannot be totally excluded.

3
ABSTRACT (German Version)
Hintergrund:
Komplexe kardiale Fehlbildungen mit vermindertem pulmonalen Blutstrom
benötigen bereits im Neugeborenenalter eine palliative Shunt-Anlage zur adäquaten
Perfusion des Lungenkreislaufs. Die Verwendung von kovalent an den Shunt
gebundenem Heparin („heparin-bonded“) Polytetrafluorethylen-Shunts (HBPS)
sollte dabei das Risiko von Graft-Verschlüssen vermindern. In dieser Studie werden
die Erfahrungen und das Outcome nach HBPS-Implantation in Patienten mit
angeborenen Herzfehlern eines Zentrums zusammengefasst.
Methoden:
Die Krankenakten von 52 Patienten, welche zwischen 2010 und 2016 einen HBPS
als aortopulmonalen Shunt erhalten haben, wurden retrospektiv analysiert. Das Alter
lag im Median bei 8 Tagen (Range: 3 – 83 Tage) und das Gewicht bei 3.2 kg (Range:
1.8 – 5.7 kg). Bis auf einen Patienten (4.0 mm) erhielten alle Patienten einen 3.5 mm
HBPS. Vierzehn Patienten (26.9%) hatten einen biventrikulär zu korrigierenden
Herzfehler und 38 Patienten (73.1%) wurden für eine univentrikuläre Palliation
vorgesehen. Als Shunt-Modifikationen wurden zentrale aorto-pulmonale Shunts
(n=35; 67.3%) und modifizierte Blalock-Taussig-Shunts (n=17; 32.7%) verwendet.
Ergebnisse:
Nach einer mittleren Nachbeobachtung von 133 Tagen (Range: 0 – 315 Tage) betrug
die Offenheitsrate der HBPS bis zur nächsten chirurgischen Intervention 90 ± 4%.
Die Frühmortalität (30 Tage) betrug 5.8% (n=3). Drei weitere Patienten verstarben
während des Krankenhausaufenthaltes. Die Todesursachen waren nicht Shunt-
assoziiert. Bei fünf Patienten trat eine HBPS-Thrombose auf, welche durch eine
Eröffnung des rechtsventrikulären Ausflusstrakts (n=2; 3.8%) oder einen Shunt-
Wechsel (n=3; 5.8%) behandelt wurde. Die HBPS-Thrombose trat entweder
intraoperativ (n=3; 5.8%), früh postoperativ nach drei Tagen (n=1; 1.9%) oder spät
postoperativ nach 41 Tagen (n=1; 1.9%) auf. Bei Patienten mit offenem HBPS
entsprach der nächste geplante chirurgische Schritt entweder einer

4
Korrekturoperation (n=10; 19.2%), einer bidirektionalen Glenn-Anastomose (n=25;
48.1%) oder einer erneuten Shunt-Anlage (n=5; 9.6%). Am Ende des Follow-up war
bei einem Patient der HBPS noch in situ. Das Überleben bis zur nächsten geplanten
Operation mit HBPS-take-down lag bei 84 ± 6% für Patienten mit univentrikulärer
Morphologie und 100% für biventrikulär korrigierbare Patienten (p=0,14).
Schlussfolgerung:
Die Verwendung von HBPS als systemisch-pulmonale Shunts erscheint sicher. Da
beim HBPS durch die kovalente Heparin-Bindung im Shunt nur ein Bestandteil der
Virchowschen Trias beeinflusst wird, können Shunt-Thrombosen, die vorwiegend
perioperativ auftreten, nicht vollständig verhindert werden.

5
1. INTRODUCTION
1.1. Palliative Shunting: A Brief Surgical History
A systemic to pulmonary artery shunt establishes pulmonary blood flow in the
context of palliative cardiac surgery. Indications for surgery exist in children with
ductal dependent or decreased pulmonary blood flow, who are not suitable for
complete repair or Glenn palliation at this stage. Moreover, children with single
ventricle physiology and obstructed systemic blood flow need systemic to pulmonary
artery shunting in the context of “classical” or Norwood-type operations.
An ideal shunt is expected to fulfil attributes like technical simple implantation,
functionality, long-term patency and easy take-down before repair. [1]
The “classic” Blalock-Taussig shunt was reported by Helen B. Taussig and Alfred
Blalock on 29 November 1944, who observed improved survival of „blue babies“
with cyanosis when the ductus Botalli was still open. In the absence of a reliable
pharmacological long-term-option to keep the duct open, division of the subclavian
artery and anastomosis to the pulmonary artery on the same side was adopted. [2, 3]
Originally a superior right antero-lateral thoracotomy was chosen as access and the
distal right subclavian artery was anastomosed to the right pulmonary artery in an
end-to-side fashion. Figure 1
Figure 1. Classic Blalock-Taussig shunt (Source:Yuan S. H, Jing H, Palliative procedures for congenital heart defects [1])

6
After performing a classic Blalock-Taussig shunt, blood flow to the ipsilateral arm is
preserved by collateral arterial vessels. This often leads to a significant reduction in
length and muscle mass of the ipsilateral arm compared to the contralateral arm. [4]
As an alternative to the “classic” Blalock-Taussig shunt, various techniques were
introduced by performing a direct anastomosis between the aorta and one pulmonary
artery. In 1946 Potts used a direct anastomosis between the descending aorta and the
left pulmonary artery. [5] Figure 2
Figure 2. Potts Anastomosis. (Source: Blanc et al, Potts shunt in patients with pulmonary hypertension [6])
Waterston used a variation of this technique in 1962 by creating a direct shunt
between the ascending aorta and right pulmonary artery through the 4th intercostal
space via right postero-lateral thoracotomy. [7] This approach was modified by
Cooley in 1966 by an antero-lateral thoracotomy. [8] A central aorto-pulmonary
shunt performing a direct anastomosis between the ascending aorta and the main

7
pulmonary artery was first published by Davidson in 1955. [9] Most of those direct
shunt variations were abandoned due to pulmonary hypertension and take down
difficulties during the next surgical procedures. Right pulmonary artery stenosis,
pulmonary hyperperfusion, pulmonary hypertension and differential pulmonary
perfusion are possible shunt related sequels before total repair. Many of these
unexpected complications were believed to be related to inaccurate initial
anastomosis of the right pulmonary artery to the aorta, later growth and later aortic
rotation. Some of these reasons, precluding later repair or further consecutive
palliation, made the Waterston shunt and Potts anastomosis disappear by the early
1980s.
Using prosthetic material, central aorto-pulmonary shunts (CAPS) were first
performed by Shumacker and Mandelbaum in 1962. [9, 10] Figure 3
Figure 3. Central aorto-pulmonary shunt using prosthetic material (Source:Yuan S. H, Jing H, Palliative procedures for congenital heart defects [1])
The advantage of this variant is an increasing patency rate in combination with a
more harmonic growth of both pulmonary arteries due to a relatively “excessive”
shunt-flow. [11, 12] A possible disadvantage of central shunting is its proximity to
the sinus of Valsalva which can lead to a significant coronary steal resulting in heart
failure or cardiac arrest. Moreover, direct sternal compression on the central shunt
may be inclined with kinking in the area of the proximal anastomosis. As an
alternative to the classical "Cobra-Head-Anastomosis” technique, Gates and Laks

8
introduced a proximal lateral-to-side anastomosis between the Gore-Tex shunt and
the ascending aorta. [11] The dorsal wall of the shunt is incised for several
millimeters and the proximal open shunt end is clipped.
Mark de Leval and McKay published in 1980 and 1981 an anastomosis between the
innominate artery and the right pulmonary artery by interposing a
polytetraflourethylen prosthesis between both vessels. This so called „modified
Blalock-Taussig shunt“ (MBTS) was initially performed on the ipsilateral side of the
aortic arch, in order to allow the use of a future classic Blalock-Taussig shunt in
growing children. [13, 14] Figure 4
Figure 4. Modified Blalock-Taussig shunt using prosthetic material (Source: Yuan S. H, Jing H, Palliative procedures for congenital heart defects [1])
Nowadays, MBTS is being used worldwide as temporary palliation with acceptable
patency rates until correction or further palliation. MBTS are usually anastomosed to
the contralateral pulmonary artery of the aortic arch.
1.2. Shunt Associated Problems and Possible Drawbacks
Beside some typical surgically associated complications such as shunt stenosis or
distortion of the pulmonary arteries [13, 15-19] shunt surgery carries a range of
possible risks. MBTS shunts can cause pseudoaneurysm formation with secondary

9
infection of the thrombotic material. [20] One the other hand, the foreign material of
MBTS can cause shunt endocarditis. [21]
Life threatening major complications like acute shunt thrombosis with sudden shunt
occlusion and imminent cardio-pulmonary resuscitation are rare. The incidence of
acute shunt thrombosis has been reported between 0-15% in different centers. [11,
22-28] A perioperative hypercoagulative state, low cardiac output and the absence of
a native intima are responsible for early shunt thrombosis, as those factors are part of
Virchow’s triad. Late shunt thrombosis usually results from progressive intimal
hyperplasia with a slow occlusion process. [21] It is less common and occurs with an
incidence of 0-5.3%. [11, 24, 26, 29, 30]
Selection of shunt size and its length are crucial for the postoperative performance. A
ratio of pulmonary artery to systemic-arterial blood flow (Qp:Qs) of approximately
1:1 is striven to be an ideal relationship, but is often difficult to achieve. Early
postoperative excessive pulmonary arterial blood flow results in pulmonary
hypercirculation with pulmonary edema and low cardiac output. [12, 31-33] In
contrast reduced systemic to pulmonary artery blood flow in the context of increased
pulmonary vascular resistance results in progressive cyanosis and possible later
organ failure and death despite adequate arterial blood pressure. As pulmonary
resistance decreases with age it counteracts patient growth for a certain time. A
balanced systemic- to pulmonary circulation is thus warranted for most patients until
the next surgical step.
1.3. Experience with "Heparin-Bonded" Shunts
Acute and late shunt-thrombosis are severe complications after palliative congenital
heart surgery. [24, 25, 34] Heparin bonded polytetrafluoroethylene shunts (HBPS)
(Propaten® Vascular Graft; W. L. Gore & Assoc, Flagstaff, Ariz) offer an
intraluminal heparin- active site, which enables binding of the clotting factor
inhibitor Antithrombin III for creation of a thrombosis-resistant surface.
Experience from vascular surgery by using HBPS show reduced platelet
deposition, decrease in inflammatory responses and a reduction of
thrombogenicity. Experience from vascular surgery suggests that HBPS may have a

10
superior outcome in the case of thromboembolic risk than uncoated grafts or
autologous venous material. A reduced morbidity and mortality has also been
described. [35-38]
The use of HBPS as systemic-to-pulmonary artery shunts in children with congenital
heart defects was described for the first time by the German Heart Center in Munich,
reporting no advantage compared to conventional shunts was reported.
Histopathologically, both types of shunt forms partial endothelialization and discrete
intimal proliferation at the time of correction or further palliation. [39]
1.4. Aim of the Study
The aim of this study was to evaluate patient survival and shunt-occlusion rates in
patients with congenital cardiac anomalies, who required systemic to pulmonary
artery shunting with HBPS in a single center. In addition, subgroup analysis of shunt
type (MBTS vs. CAPS) and cardiac morphology (univentricular vs. biventricular)
was scrutinized regarding their influence on HBPS-performance.

11
2. MATERIAL AND METHODS
2.1. Patients
All patients, who received HBPS between January 2010 and December 2016, were
retrospectively reviewed. Inclusion criteria were age under 3 months, anterior
sternotomy approach and HBPS as initial palliative surgical treatment. Patients were
categorized with respect to their cardiac morphology whether they went the
univentricular or biventricular pathway.
2.2. Surgical Technique
All cardiac procedures were performed via median sternotomy. The pulmonary
arteries and ductus arteriosus were dissected and the anatomic structures evaluated.
In patients with hypoplastic left heart syndrome, it is our institutional policy to
perform Norwood procedures with a right ventricle to pulmonary artery conduit
(“Sano-Shunt”/non-HBPS). These patients were not included in this analysis.
Variants with a morphologic left ventricle, however, were palliated with MBTS. The
decision in other than Norwood patients to proceed with a MBTS or CAPS is made
according to the position, size, and anatomic relation of the pulmonary arteries to the
aorta and its branching patterns. [40] CAPS and MBTS were performed as
previously described. For MBTS, an obliquely fashioned end of the HBPS was
sutured end-to-side to the innominate artery. The straight distal end of the graft was
anastomosed to the right or left pulmonary artery depending on arch and PA-
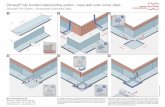
anatomy. [27] Figure 5A For CAPS, distal end-to-side anastomosis between shunt
and main pulmonary artery, and proximal side-to-side anastomosis between shunt
and aorta were performed. The open end of the shunt was trimmed and clipped close
to the proximal anastomosis after de-airing. [11] Figure 5B
If necessary, cardiopulmonary bypass was admitted. Moderate hypothermia (32-
35°C) was used for standard shunt operations without additional procedures.
Antegrade modified blood cardioplegia was administered if cardioplegic arrest was
necessary. Septectomy in univentricular patients was performed to improve intra-
cardiac mixing at the atrial level. Modified Norwood procedures using MBTS were

12
performed in moderate hypothermia (25-28°C) with regional cerebral perfusion.
Correction of total anomalous pulmonary venous drainage was performed under deep
hypothermia (18°C) with circulatory arrest. After weaning from bypass modified
ultrafiltration was carried out.
Figure 5 AB. Modified Blalock-Taussig shunt (A) and central aorto-pulmonary shunt with proximal end-to-side technique (B).
2.3. Follow-up
Follow-up was accomplished by routine control echocardiography or direct contact
with the referring cardiologist, until July 31st 2017. All patients with systemic to
pulmonary artery shunt are scheduled for cardiac catheterization at the age of 3
months.
Shunt patency was defined as “native” open graft until estimated next surgical
treatment, which was either corrective surgery or bidirectional Glenn procedure.
Additionally, in patients who were not eligible for those two procedures despite open
graft, elective shunt replacement was scheduled whenever patient outgrowth was
suspected.
Shunt thrombosis was managed according to anatomical features by intervention or
surgery. The former included balloon dilatation and stent placement if necessary. The

13
latter comprised new shunting with CAPS, MBTS, right ventricular to pulmonary
artery conduit, or patch enlargement of the right ventricular outflow tract.
2.4. Statistical Analysis
Data were collected using Microsoft Excel 2010. Analysis was performed with SPSS
21.00 (SPSS Inc., Chicago, IL, USA). Descriptive data for continuous variables are
reported as median with ranges or mean ± standard deviation. Categorical variables
are presented as numbers or percentages. Risk adjustment was stratified according to
the Aristotle and RACHS score. Primary end-points were calculated by X²-test and
the Kaplan-Meier method (log-rank) which included survival until the planned next
procedure, and patency of HBPS. Statistical significance was established at a
p-value<0.05.

14
3. RESULTS
3.1. Patient Characteristics and Operative Data
Fifty-two patients with HBPS were identified, of whom all except 3 were operated
on cardiopulmonary bypass. Thirty-five patients received CAPS (67.3%) and 17
patients MBTS (32.7%). Size of HBPS was 3.5 mm in 51 patients (98.1%) and 4 mm
in 1 patient (1.9%). The patient characteristics are summarized in Table 1 and
operative data in Table 2.
Table 1. Patient Characteristics
Value % Median Range
Male 29 55.7
Body weight: (kg) 3.2
3.2 1.8 - 5.72
Age: (days) 8
8 3 - 83
Univentricular morphology
HLHS + variants 13 25
HRHS 19 36.5
Heterotaxy 6 11.5
Biventricular morphology
TOF / DORV 6 11.5
Pulmonary atresia + VSD 5 9.6
TGA + pulmonary stenosis 3 5.8
DORV: double outlet right ventricle; HLHS: hypoplastic left heart syndrome; HRHS: hypoplastic
right heart syndrome; TGA: transposition of great arteries; TOF: tetralogy of Fallot; VSD: ventricular
septal defect

15
Table 2. Operative Data
N % Median Range
Central aorto-pulmonary shunt (CAPS) 35 67.3
isolated 23 44.2
TAPVD correction 2 3.8
Septectomy 7 13.5
Pulmonary artery reconstruction 3 5.8
Modified Blalock-Taussig shunt (MBTS) 17 32.7
isolated 3 5.8
Septectomy 1 1.9
Norwood I 13 25
Shunt size
3.5 mm 51 98.1
4 mm 1 1.9
Aristotle-Score
6.8 6.3-15
RACHS
3 3-6
Surgery time (minutes)
255.5 112-574
Bypass time (minutes)
68 23-360
Aortic crossclamp time (minutes)
37 8-118
Temperature (° C )
32.5 19.2-36.4
RACHS: risk adjustment for congenital heart surgery

16
Two patients initially scheduled for biventricular repair went the univentricular
pathway. In 2 patients the decision for further palliation was made during the
second step operation due to straddling mitral valve in a patient with corrected
transposition and pulmonary atresia originally planned for Senning/ Rastelli, and
due to “remote” ventricular septal defect in a patient with double outlet right
ventricle and malposition of great arteries. In addition, one patient with corrected
transposition and pulmonary atresia, who received bidirectional Glenn at second
step was referred to further “1 and 1/2 repair” and was classified to biventricular
patients. Thus in total, 14 patients (26.9%) were stratified to be biventricular and
38 patients (73.1%) to have functionally univentricular morphology.
3.2. Survival
Early mortality (30 days) was 5.8% (n=3). Another 3 patients died during their
hospital stay. Hospital mortality was 0% in biventricular patients and 11.5% (n=6)
in univentricular patients (p = 0.27). Six of the latter died with HBPS in situ, all non-
shunt related. Causes of death were heart failure (n=5) and sepsis (n=1).
Median duration until next palliative or corrective surgical procedure was 141 days
(range: 0 - 463). At the end of follow-up, 1 patient had HBPS still in situ.
Estimated second procedure included corrective surgery (n=10; 19.2%), bidirectional
Glenn (n=25; 48.1%) and shunt replacement (n=5; 9.6%). Reasons for new shunting
despite open HBPS (univentricular n=4; 7.7%, biventricular n=1; 1.9%) were
intraoperative hemodynamic instability (n=1; 1.9%), non-eligibility for biventricular
repair (n=1; 1.9%) or bidirectional Glenn (n=1; 1.9%), pulmonary artery distortion
(n=1; 1.9%) and bronchial obstruction (n=1; 1.9%).
A flow-chart until next surgical treatment including take-down of HBPS is shown in
Figure 6.

17
Figure 6. Flow chart of HBPS treatment algorithm. CAPS: central aorto-pulmonary shunt; MTBS: modified Blalock-Taussig shunt; RVOT: right ventricular outflow tract

18
Survival until planned second procedure in patients with biventricular morphology
was 100% and in patients with univentricular morphology 84 ± 6% (p = 0.14).
Figure 7
Figure 7. Kaplan-Meier survival

19
3.3. Shunt Patency
Shunt patency was 90 ± 4% after a median duration of 133 days (range: 0 - 315
days). There was no significant difference between uni- and biventricular
patients regarding the freedom from shunt-thrombosis (biventricular:
85 ± 1% vs. single ventricle: 92 ± 5%; p=0.48). Incidence of early shunt
thrombosis in univentricular patients was 5.3% (n=2) and in biventricular 14.3%
(n=2) (p = 0.61), whereas late thrombosis was 2.6 % which occurred in 1
univentricular patient. Figure 8
Figure 8. Kaplan-Meier freedom from shunt thrombosis until next planned surgical treatment.

20
When discriminating between CAPS and MBTS, shunt patency was 88 ± 6% and
94 ± 6% (p=0.55), respectively. Incidence of early shunt thrombosis with CAPS was
8.6% and with MBTS 5.9%. Late thrombosis was rare and occured in one patient with
CAPS (n=1; 2.9%/ p = 1.00). Figure 9
Figure 9. Kaplan-Meier freedom from shunt thrombosis until next planned surgical treatment compared between distinct shunt modifications. CAPS: central aorto-pulmonary shunt; MTBS: modified Blalock-Taussig shunt
Shunt revision due to subtotal occlusion was performed in 5 patients (9.6%) and was
necessary either intraoperatively (n=3), early postoperatively (n=1) after 3 days on
ICU, or late post operatively (n=1) after 32 days. Data regarding shunt thrombosis are
summarized in Table 3.

21
Table 3. Shunt Thrombosis
Group Weight Age
Shunt
size Secondary
procedure
Onset of
Thrombosis Outcome
(kg) (days) (mm) (days)
Intraoperative shunt thrombosis after:
1. CAPS single ventricle 3.7 18 3.5 CAPS 0 discharged after Glenn
2. MTBS + septectomy single ventricle 2.6 5 3.5 CAPS 0 discharged after Glenn
3. CAPS biventricular 2.4 8 3.5 RVOT-
opening 0 discharged after correction
Postoperative shunt thrombosis after:
1. CAPS (3 days) biventricular 3.6 9 3.5
RVOT-
opening 3 discharged after correction
Late shunt thrombosis:
1.CAPS + TAPVD correction single ventricle 3.2 14 3.5 CAPS 41 discharged after Glenn
CAPS: central aorto-pulmonary shunt; MTBS: modified Blalock-Taussig shunt; TAPVD: Total Anomaly Venous Drainage; RVOT: right ventricular outflow tract.

22
Subtotal graft occlusion was managed by shunt resection and patch enlargement of
the right ventricular outflow tract in biventricular patients (n=2), and shunt revision
in univentricular patients (n=3). A resected and opened graft with thrombotic
material is shown in Figure 10.
Figure 10. Intraoperative shunt thrombosis in a resected HBPS

23
4. DISCUSSION
This study demonstrates outcomes after placement of HBPS in the context of
palliative congenital heart surgery. Cardiac morphology included patients with
univentricular and biventricular cardiac pathology, both eligible for further corrective
or palliative surgery.
4.1. Survival
Survival until the next elective procedure in biventricular patients was excellent
(100%). However in patients with univentricular morphology, outcome was
significantly less promising (84%). Patient attrition was not shunt-related and mainly
influenced by the underlying disease including hypoplastic left heart
complex/syndrome and heterotaxy. [41]
Palliative shunt surgery is reported with early mortalities between 0% and 18.2%
[11, 12, 22, 23, 27, 28, 32, 33, 42-45], and late mortalities between 3.8% and 19%.
[32, 33, 46] Reasons for unfavorable outcome were excessive pulmonary flow,
sepsis, and arrhythmia or shunt thrombosis.[12, 33, 46] Mortality early and late after
shunt operations is significant, despite being a non-complex surgical procedure.
Bove et al reported an in-hospital-mortality of 8.7% and later interstage mortality of
5.1% among 150 MBTS-patients operated between 1995 and 2013. [47] Fenton et al
reported an interstage mortality of 7.1% in biventricular patients and 19% in patients
with univentricular morphology. The authors pointed out, that autopsy-proven shunt
thrombosis was one of the leading causes of interim sudden death. [46] In order to
reduce the risk of shunt thrombosis, biologic material like saphenous venous
homograft for MTBS has been introduced by Erez et al. in 17 infants less than 3
kilograms. Hospital mortality for the entire cohort was 6.3% and survival rates until
shunt take-down 58% in the univentricular group and 90% in the biventricular group.
[42] Alsoufi et al reported significantly higher hospital mortality in univentricular
patients but comparable survival until next elective procedure when compared to
biventricular patients. [44] Other groups were not able to show a significant effect for
univentricular morphology as predictor of death or shunt dysfunction. [12, 27, 48]

24
4.2. Shunt Patency
Incidence of early and late shunt thrombosis was 7.6% and 1.9%, respectively. The
observed results are in accordance with the experience of other studies concerning
systemic-to-pulmonary shunting, where early and late shunt thrombosis ranged
between 0-15 % [11, 22-28] and 0-5.3% [11, 24, 26, 29, 30], respectively.
Shunt patency in our cohort was 90 ± 4% with no significant difference between uni-
and biventricular patients. This seems different to some other studies, in which shunt
thrombosis seemed to occur more often in univentricular patients (5.5-18.1%) when
compared to biventricular patients (4.7-7.1%). [27, 46]
One possible reason for shunt thrombosis in our cohort was reduced HBPS blood
flow, as a consequence of continuous low output syndrome after weaning from
cardiopulmonary bypass, or concurrent flow due to sustained antegrade perfusion of
the pulmonary artery via the RVOT. Stasis of blood flow enhances thrombosis as a
well-known part of Virchow’s triad. [39]
There was no significant difference between CAPS to MBTS regarding their patency
rate. When looking at other studies with selective use of either procedure, this
finding is confirmed by other authors, where early shunt thrombosis by using CAPS
0-16.7 % [11, 23, 24] and with MBTS between 5 -14.9% [22, 24-28], whereas late
thrombosis was 0% [11] and 0-5.3%. [24, 26, 29, 30]
All patients with shunt thrombosis could be successfully referred to further palliative
surgery. In one patient balloon dilatation of subtotal late shunt thrombosis was
performed as a bridge to shunt replacement. Five additional patients needed shunt
intervention for anatomical reasons or successive narrowing of the shunt, which
might be related to aggravating intimal hyperplasia. [39] Other studies reported that
9.7-17% of their patients needed catheter-reintervention after systemic-to-pulmonary
shunting. [31, 34]
4.3. HBPS
Studies from vascular surgery reported that heparin-bonded vascular grafts provided
improved patency rates and limb salvage in patients with peripheral vascular disease.

25
[38] Daenens et al. reported a similar 1-2 years patency rate when comparing
heparin-bonded grafts to autologous saphenous vein grafts. [49] Kirkwood et al.
suggested that heparin-bonded vascular grafts should be the conduit of choice for all
prosthetic bypasses. [37]
There is a limited number of reports in the literature regarding the use of HBPS in
the palliative setting of congenital heart surgery for newborns. In a small series,
Hörer et al. compared HBPS to classic polytetrafluorethylene shunts and revealed
equally good clinical outcomes for patients with both types of shunts. The
histopathological workup revealed a faster process of endothelialization with HBPS
within the first 30 days, which may prevent the patient from shunt thrombosis in the
early interim period. However, the process of intimal proliferation was not affected
by HBPS, still exposing the patient to the risk of late shunt thrombosis. [39]
4.4. Limitations
Limitations of the study are inherent to the retrospective nature of data retrieval.
Historical influences on patients outcome related to improvements in surgical
techniques and intensive care protocols over the study period cannot be excluded.
4.5. Conclusion
The use of HBPS is safe and seems to warrant systemic to pulmonary perfusion
sufficiently. Despite the covalent binding of Heparin in the HBPS inner layer, Shunt-
thrombosis cannot be excluded totally and occurs predominantly early. However,
those patients can be transferred relatively safe to further palliative treatment,
indicating a delay in the process of shunt occlusion by using HBPS.

26
5. REFERENCES
1. Yuan, S.M. and H. Jing, Palliative procedures for congenital heart defects.
Arch Cardiovasc Dis, 2009. 102(6-7): p. 549-57.
2. Blalock, A. and H.B. Taussig, Landmark article May 19, 1945: The surgical
treatment of malformations of the heart in which there is pulmonary stenosis
or pulmonary atresia. By Alfred Blalock and Helen B. Taussig. JAMA, 1984.
251(16): p. 2123-38.
3. Blalock, A., The surgical treatment of congenital pulmonic stenosis. Science,
1947. 105(2738): p. 633.
4. Harris, A.M., N. Segel, and J.M. Bishop, Blalock-Taussig Anastomosis for
Tetralogy of Fallot. A Ten-to-Fifteen Year Follow-Up. Br Heart J, 1964. 26:
p. 266-7.
5. Potts, W.J., S. Smith, and S. Gibson, Anastomosis of the aorta to a pulmonary
artery in certain types of congenital heart disease. Case Rep Child Meml
Hosp Chic, 1946. 5(12): p. 704-18.
6. Blanc, J., P. Vouhe, and D. Bonnet, Potts shunt in patients with pulmonary
hypertension. N Engl J Med, 2004. 350(6): p. 623.
7. Waterston, D.J., [Treatment of Fallot's tetralogy in children under 1 year of
age]. Rozhl Chir, 1962. 41: p. 181-3.
8. Cooley, D.A. and G.L. Hallman, Intrapericardial aortic-right pulmonary
arterial anastomosis. Surg Gynecol Obstet, 1966. 122(5): p. 1084-6.
9. Davidson, J.S., Anastomosis between the ascending aorta and the main
pulmonary artery in the tetralogy of Fallot. Thorax, 1955. 10(4): p. 348-50.
10. Shumacker, H.B., Jr. and I. Mandelbaum, Ascending aorticpulmonary artery
shunts in cyanotic heart disease. Surgery, 1962. 52: p. 675-8.
11. Gates, R.N., H. Laks, and K. Johnson, Side-to-side aorto-Gore-Tex central
shunt. Annals of Thoracic Surgery, 1998. 65(2): p. 515-516.
12. Barozzi, L., et al., Side-to-side aorto-GoreTex central shunt warrants central
shunt patency and pulmonary arteries growth. Ann Thorac Surg, 2011. 92(4):
p. 1476-82.

27
13. McKay, R., et al., Postoperative angiographic assessment of modified
Blalock-Taussig shunts using expanded polytetrafluoroethylene (Gore-Tex).
Ann Thorac Surg, 1980. 30(2): p. 137-45.
14. de Leval, M.R., et al., Modified Blalock-Taussig shunt. Use of subclavian
artery orifice as flow regulator in prosthetic systemic-pulmonary artery
shunts. J Thorac Cardiovasc Surg, 1981. 81(1): p. 112-9.
15. Fenchel, G., et al., Early and late results of the modified Waterston shunt with
PTFE grafts for palliation of complex congenital cyanotic heart disease in
neonates. Thorac Cardiovasc Surg, 1991. 39(5): p. 268-72.
16. Ni, B., et al., "One-stop" hybrid approach to surgical correction of Tetralogy
of Fallot with a 37-year left classic Blalock-Taussig shunt. Int J Cardiol,
2016. 223: p. 4-6.
17. Daehnert, I., M. Wiener, and M. Kostelka, Covered stent treatment of right
pulmonary artery stenosis and Waterston shunt. Ann Thorac Surg, 2005.
79(5): p. 1754-5.
18. Hovis, I.W., N.J. Sutton, and R.H. Pass, Intervening for RPA stenosis
following Waterston shunt: Importance of anatomical definition of the
coronary arteries. Catheter Cardiovasc Interv, 2014. 83(4): p. 591-4.
19. Singh, A.K., Transection of the aorta for repair of pulmonary artery branch
stenosis after creation of a Waterston shunt. Cardiovasc Dis, 1981. 8(4): p.
550-554.
20. Okada, N., H. Murayama, and H. Hasegawa, Optimal Surgical Management
Using a Classic Blalock-Taussig Shunt for an Infected Pseudoaneurysm After
a Modified Blalock-Taussig Shunt Procedure. Ann Thorac Surg, 2016.
101(5): p. 1992-5.
21. Wells, W.J., et al., Obstruction in modified Blalock shunts: a quantitative
analysis with clinical correlation. Ann Thorac Surg, 2005. 79(6): p. 2072-6.
22. Alkhulaifi, A.M., et al., Systemic pulmonary shunts in neonates: early clinical
outcome and choice of surgical approach. Ann Thorac Surg, 2000. 69(5): p.
1499-504.
23. Kim, H., et al., A central shunt to rehabilitate diminutive pulmonary arteries
in patients with pulmonary atresia with ventricular septal defect. J Thorac
Cardiovasc Surg, 2015. 149(2): p. 515-20.

28
24. Anderson, B.R., et al., The effects of postoperative hematocrit on shunt
occlusion for neonates undergoing single ventricle palliation. J Thorac
Cardiovasc Surg, 2016.
25. Guzzetta, N.A., et al., In-hospital shunt occlusion in infants undergoing a
modified blalock-taussig shunt. Ann Thorac Surg, 2013. 96(1): p. 176-82.
26. Gedicke, M., et al., Risk factors for acute shunt blockage in children after
modified Blalock-Taussig shunt operations. Heart Vessels, 2010. 25(5): p.
405-9.
27. Dirks, V., et al., Modified Blalock Taussig shunt: a not-so-simple palliative
procedure. Eur J Cardiothorac Surg, 2013. 44(6): p. 1096-102.
28. Kucuk, M., et al., Risk Factors for Thrombosis, Overshunting and Death in
Infants after Modified Blalock-Taussig Shunt. Acta Cardiol Sin, 2016. 32(3):
p. 337-42.
29. Swain, S.K., et al., Neonatal Blalock-Taussig shunt: technical aspects and
postoperative management. Asian Cardiovasc Thorac Ann, 2008. 16(1): p. 7-
10.
30. Mullen, J.C., G. Lemermeyer, and M.J. Bentley, Modified Blalock-Taussig
shunts: to heparinize or not to heparinize? Can J Cardiol, 1996. 12(7): p. 645-
7.
31. Myers, J.W., et al., Outcomes of systemic to pulmonary artery shunts in
patients weighing less than 3 kg: analysis of shunt type, size, and surgical
approach. J Thorac Cardiovasc Surg, 2014. 147(2): p. 672-7.
32. Chowdhury, U.K., et al., Criterions for selection of patients for, and results
of, a new technique for construction of the modified Blalock-Taussig shunt.
Cardiol Young, 2006. 16(5): p. 463-73.
33. Bao, M., et al., Central shunt procedures for complex congenital heart
diseases. J Card Surg, 2014. 29(4): p. 537-41.
34. O'Connor, M.J., et al., Early systemic-to-pulmonary artery shunt intervention
in neonates with congenital heart disease. J Thorac Cardiovasc Surg, 2011.
142(1): p. 106-12.
35. Begovac, P.C., et al., Improvements in GORE-TEX vascular graft
performance by Carmeda BioActive surface heparin immobilization. Eur J
Vasc Endovasc Surg, 2003. 25(5): p. 432-7.

29
36. Golchehr, B., et al., Clinical Outcome of Isolated Popliteal Artery Aneurysms
Treated with a Heparin-bonded Stent Graft. Eur J Vasc Endovasc Surg, 2016.
52(1): p. 99-104.
37. Kirkwood, M.L., et al., Lower limb revascularization for PAD using a
heparin-coated PTFE conduit. Vasc Endovascular Surg, 2011. 45(4): p. 329-
34.
38. Bosiers, M., et al., Heparin-bonded expanded polytetrafluoroethylene
vascular graft for femoropopliteal and femorocrural bypass grafting: 1-year
results. J Vasc Surg, 2006. 43(2): p. 313-8; discussion 318-9.
39. Horer, J., et al., A Comparative Histopathological Study of Heparin Coated
and Uncoated Polytetrafluoroethylene Shunts in Children With Congenital
Heart Defect. World J Pediatr Congenit Heart Surg, 2014. 5(3): p. 385-390.
40. Brink, J., et al., Neonatal pulmonary artery reconstruction during shunting to
treat and prevent juxtaductal coarctation. Ann Thorac Surg, 2015. 99(2): p.
641-7.
41. Gaynor, J.W., et al., Long-term outcome of infants with single ventricle and
total anomalous pulmonary venous connection. J Thorac Cardiovasc Surg,
1999. 117(3): p. 506-13; discussion 513-4.
42. Erez, E., et al., Outcome in infants less than 3 kilograms for placement of
saphenous venous homografts as systemic-to-pulmonary arterial shunts.
Cardiol Young, 2008. 18(4): p. 386-91.
43. Petrucci, O., et al., Risk factors for mortality and morbidity after the neonatal
Blalock-Taussig shunt procedure. Ann Thorac Surg, 2011. 92(2): p. 642-51;
discussion 651-2.
44. Alsoufi, B., et al., Factors affecting death and progression towards next stage
following modified Blalock-Taussig shunt in neonates. Eur J Cardiothorac
Surg, 2016. 50(1): p. 169-77.
45. Fenton, K.N., et al., Interim mortality in pulmonary atresia with intact
ventricular septum. Ann Thorac Surg, 2004. 78(6): p. 1994-8; discussion
1998.
46. Fenton, K.N., et al., Interim mortality in infants with systemic-to-pulmonary
artery shunts. Ann Thorac Surg, 2003. 76(1): p. 152-6; discussion 156-7.

30
47. Bove, T., et al., Disease-specific outcome analysis of palliation with the
modified Blalock-Taussig shunt. World J Pediatr Congenit Heart Surg, 2015.
6(1): p. 67-74.
48. Chittithavorn, V., et al., Risk factors for in-hospital shunt thrombosis and
mortality in patients weighing less than 3 kg with functionally univentricular
heart undergoing a modified Blalock-Taussig shuntdagger. Interact
Cardiovasc Thorac Surg, 2017.
49. Daenens, K., et al., Heparin-bonded ePTFE grafts compared with vein grafts
in femoropopliteal and femorocrural bypasses: 1- and 2-year results. J Vasc
Surg, 2009. 49(5): p. 1210-6.

31
6. ABBREVIATIONS
CAPS central-aorto-pulmonary shunt
DORV double outlet right ventricle
HBPS heparin-bonded polytetra-fluorethylen shunts
HLHS hypoplastic left heart syndrome
HRHS hypoplastic right heart syndrome
MBTS modified Blalock-Taussig shunt
RACHS risk adjustment for congenital heart surgery
RVOT right ventricular outflow tract
TAPVD total anomalous pulmonary venous drainage
TGA transposition of great arteries
TOF tetralogy of Fallot
VSD ventricular septal defect

32
7. LIST OF FIGURES
Figure 1. Classic Blalock-Taussig Shunt
Figure 2. Potts Anastomosis
Figure 3. Central aorto-pulmonary shunt using prosthetic material
Figure 4. Modified Blalock-Taussig shunt using prosthetic material
Figure 5.
A. modified Blalock-Taussig-shunt
B. central aorto-pulmonary shunt with proximal end-to-side technique
Figure 6. Flow chart of HBPS treatment algorithm
Figure 7. Kaplan-Meier survival
Figure 8. Kaplan-Meier freedom from shunt thrombosis until next planned
surgical treatment
Figure 9. Kaplan-Meier freedom from shunt thrombosis compared between
distinct shunt modifications until next planned procedure
Figure 10. Intraoperative shunt thrombosis in a resected HBPS

33
8. LIST OF TABLES
Table 1. Patient Characteristics
Table 2. Operative Data
Table 3. Shunt Thrombosis

34
9. ACKNOWLEDGEMENTS
I would sincerely like to thank Professor Dr. med. Robert Cesnjevar for the
opportunity to do research in his department and the continuous support and
guidance.
I would like to honourly thank PD Dr. med. André Rüffer for his supervision,
patience, and time.
I would like to kindly thank the team of the Department of Pediatric Cardiac Surgery
in Erlangen, Dr. med. Ariawan Purbojo, Robert Blumauer, MD, for supporting my
scientific work.
Professor Jürgen von der Emde for the invitation to Germany.
My parents, Endang Ambar Rukminingsih, SP.d and Dasaad Achsany, M.B.A for all
supports. My sisters and their families, Shintia Adny Noviarukmi, S.H, M.Kn,
Mayang Adny Puspitaning Dewi, S.AB, Ihwan Handy Rosiyanto, M.D, FIHA,
Aribowo, S.T, M.T.
Mrs. Monika Prowosnik, Mrs. Simone Marten, Mrs. Natalie Seifert, Mr. Frank
Münch, Mrs. Manuela Bader, Mrs. Sabrina Mandelkow, Ms. Teresa Adt, Ms.
Johanna Jahnke, Ms. Vanessa Maley, for helping me as long as I have been working
here.

35
10. DISCLAIMER
I certify that my Dissertation is my own work and an original report of my research.
Part this work has been presented at the 7th World Congress of Pediatric Cardiology
and Cardiac Surgery, Barcelona, Spain, 2017.
A journal publication of this work is in progress and will be submitted, soon.
Erlangen, 16.08.2017
Yuletta Adny Ambarsari