Second-harmonic generation microscopy for assessment of ......Second-harmonic generation microscopy...
Transcript of Second-harmonic generation microscopy for assessment of ......Second-harmonic generation microscopy...

lable at ScienceDirect
Biomaterials 53 (2015) 659e668
Contents lists avai
Biomaterials
journal homepage: www.elsevier .com/locate/biomater ia ls
Second-harmonic generation microscopy for assessment ofmesenchymal stem cell-seeded acellular dermal matrix in wound-healing
Qiannan Wang a, Ying Jin a, *, Xiaoyuan Deng a, b, **, Hanping Liu a, Hongwen Pang c,Panpan Shi a, Zhigang Zhan a
a MOE Key Laboratory of Laser Life Science, College of Biophotonics, South China Normal University, Guangzhou, Guangdong, Chinab Research Resources Center, South China Normal University, Guangzhou, Guangdong, Chinac Guangzhou Institutes of Biomedicine and Health, Chinese Academy of Sciences, Guangzhou, Guangdong, China
a r t i c l e i n f o
Article history:Received 15 September 2014Received in revised form3 March 2015Accepted 4 March 2015Available online 24 March 2015
Keywords:Wound healingAcellular dermal matrix (ADM)Mesenchymal stem cells (MSCs)Two-photon fluorescence (TPF) microscopySecond-harmonic generation (SHG)microscopy
* Corresponding author. Tel.: þ86 13610047142.** Corresponding author. MOE Key Laboratory of LBiophotonics, South China Normal University, GuaTel.: þ86 13794340045.
E-mail addresses: [email protected] (Y. Jin), xyd
http://dx.doi.org/10.1016/j.biomaterials.2015.03.0110142-9612/© 2015 Elsevier Ltd. All rights reserved.
a b s t r a c t
Direct intra-skin injection of mesenchymal stem cells (MSCs) and the use of biomaterial scaffolds forgrafts are both promising approaches of skin wound repair, however they still cannot generate skin thatcompletely resembles the natural skin structures. In this study, we combined these two approaches byusing acellular dermal matrix (ADM) recellularized with MSCs to repair cutaneous wounds in a murinemodel and two-photon fluorescence (TPF) microscopy and second-harmonic generation (SHG) micro-scopy to assess the effects of this therapy on wound healing. Bone marrow-derived mesenchymal stemcells (BM-MSCs) were tagged with GFP and seeded into ADM (ADM-MSC) via MSC and ADM co-culture.ADM-MSC, ADM or saline was applied to murine excisional skin wounds and wound-healing wasevaluated by histological examination on days 7, 14, 21 and TFP microscopy on days 1, 3, 5 and 21 post-treatment. ADM-MSC promoted healing significantly more than treatment with ADM or saline alone, asit led to substantial neovascularization and complete skin appendage regeneration. Furthermore, theSHG microscopic imaging technique proved to be a useful tool for monitoring changes in the collagennetwork at the wound site during the healing process and assessing the effects of different therapies.
© 2015 Elsevier Ltd. All rights reserved.
1. Introduction
Full-thickness skin wounds can result from a variety of injuries,such as acute trauma, chronic ulcers, and extensive burns, and cancause numerous physiological and functional problems. The idealtreatment should provide a coverage that supports the repair ofskin structure and restoration of skin function. Towards this goal,many studies have sought to develop biomaterials that not onlyresemble the natural skin tissue architecture, but also facilitate cellcolonization [1].
Acellular dermal matrices (ADMs) are the native extracellularmatrices which are derived from human or animal skin by
aser Life Science, College ofngzhou, Guangdong, China.
[email protected] (X. Deng).
removing the epidermis and all dermal cells. ADMs are widely usedfor skin reconstruction and surgical applications (burn injuries,ulcers and post trauma surgery) [2] as they can be rapidly inte-grated into the wound tissues with favorable biocompatibility [3].In the applications of ADMs for different wound healing, ADMsusually act as a scaffold for host cellular infiltration and undergoprogressive remodeling to form functional tissue without immu-nogenic response [4]. Collagen proteins are the main component ofthe acellular scaffolds and other minor extracellular matrix (ECM)proteins such as fibronectin, laminin and vimentin are alsoincluded [2].
Another strategy for improving skin regeneration in cutaneouswounds is to use stem cell-based therapies. Recent studies haveshown that mesenchymal stem cells (MSCs) have great regenera-tive potential, and their multipotentiality and the ability to prolif-erate in vitro for long periods of time [5] are also advantageous foruse in therapy. The mechanisms of MSCs enhancing tissue repairare complex, as MSCs can participate in all three phases (inflam-mation, proliferation and remodeling) of skin regeneration [6,7].

Q. Wang et al. / Biomaterials 53 (2015) 659e668660
Many studies have suggested that MSCs can function as vascularpericytes [8] and contribute to tissue repair by secreting factors thatcan stimulate the proliferation and differentiation of endogenousprogenitors, decrease inflammatory reactions and promote angio-genesis [9,10]. Others reported that MSCs cultured in vitro ondermal equivalents acquired the phenotype and function of myo-fibroblasts, leading to ECM remodeling and matrix contraction[11e13]. MSC-seeded ADM is considered to be a promising strategyfor accelerating wound healing [7,14], but it has not been exten-sively tested experimentally.
Thus far most of the research on MSC activity and collagenremodeling during the wound healing process has been donein vitro or in biopsied animal tissues, due to a lack of feasible meansto directly monitor the dynamic interaction between MSCs and theECM remodeling in wound site during the healing process. Usingnonlinear microscopic optical imaging techniques may resolve thisissue since cell activities can be traced and collagen structure can bemonitored intravitally [15,16]. Two-photon fluorescence (TPF) andsecond-harmonic generation (SHG) are two well-known nonlinearoptical phenomena that have been utilized in microscopic imagingof tissues, namely the TPF microscopy and SHG microscopy,respectively. TPF and SHG rely on different nonlinear light-matterinteraction mechanisms, but can usually be taken together togenerate combined images in a same optical microscopic imagingsystem [17,18]. In TPF microscope framework, only fluorophoreswithin the focal plane can be excited by simultaneous (within10�16 s) absorption of two photons. This restricts the fluorescenceemission to the focal plane, thus greatly reducing out-of-planephotobleaching, phototoxicity and ultimately achieving intrinsicthree-dimensional resolution. In SHG microscopy, as an intenseinput laser light passes through non-centrosymmetric molecules, itinduces a second-order nonlinear polarization in those molecules.As a result, an emission light with exactly twice the frequency (halfthe wavelength) of input is generated. SHG signals are tissue-intrinsic and do not require extra extrinsic dyes, thus SHG micro-scopy fully preserves the normal function of biological systems. Thefibrous collagen type I in skin tissue has been proved to be thesource of strong intrinsic SHG signals [17,19]. Both TPF and SHGhave the ability to construct 3D images of specimens, and since thenear-infrared femtosecond pulse light is adopted, these nonlinearmicroscopic imaging methods have gained the ability of imagingthick tissues while eliciting minimal damages on them. Naturally,TPF microscopy and SHG microscopy have been widely used forvisualization of cells, tissues and organisms [18,20,21].
In the current study, ADM was seeded with MSCs and was thenused to treat full-thickness skin defects. Thewound healing processwas examined with TPF and SHG imaging to dynamically trace theactivities of MSCs and collagen remodeling. The results indicatethat MSCs seeded on ADM scaffold as a wound bed sheet canpromote the dermal structural regeneration, angiogenesis, re-epithelialization and collagen remodeling, and ultimately accel-erate the healing of murine cutaneous wounds.
2. Materials and methods
2.1. Preparation of ADM scaffolds
Skin from five-week-old male BALB/c mice was used to prepare ADM scaffolds.The mice were euthanized via cervical dislocation. The dorsal hair was shaved andpieces of 3 � 5 mm2 full-thickness skin were harvested. The skin tissues weretreated with 0.25% Dispase (Aoboxing, Beijing, China) at 4
�C for 48 h to separate the
epidermis and then immersed in PBS supplemented with 0.3% Triton- X-100, 0.25%sodium deoxycholate and 0.02% EDTA under continuous oscillation, at 37
�C for 48 h
in order to remove the cellular components from the matrix. The decellularizedscaffolds were then treated with a fat digestion solution of chloroform andmethanol(v/v ¼ 1:1) for 1e2 h and washed three times in PBS. Finally, the scaffolds weresterilized in 70% ethanol for 30 min and washed three times with sterile PBS. TheADM scaffolds were stored in DMEM medium at 4
�C till use.
2.2. SEM (scanning electron microscope) imaging of ADM
Decellularized ADM scaffolds were fixed in 2.5% gluaraldehyde at 4 �C for at least24 h. Scaffolds were then dehydrated by immersion in an ascending ethanol series(30%, 50%, 75%, 90%, and 100%), treated twice with isoamylacetate, critical pointdried and sputter-coated with a 30 nm gold layer. Samples were imaged using ascanning electron microscope (Zeiss Ultra 55, Carl Zeiss, Jena, Germany) in order toshow the collagen organization and construction of the ADM scaffolds.
2.3. Seeding of MSCs on ADM
C57BL/6 mouse bone marrow mesenchymal stem cells (mBMSCs, MUCMX-01101, GFP-tagged) were purchased from Cyagen Biosciences, Inc. (Guangzhou,China), and cultured in OriCellTM mouse MSC Growth Medium (MUCMX-90011,Cyagen Biosciences, Inc.) in a humidified incubator at 37
�C with 5% CO2. Round
pieces of ADM scaffolds (6 mm in diameter) were acquired via biopsy punches andplaced in a 48-well plate (one piece per well) with the papillary dermis side facingupward. ADM scaffolds were incubated overnight in freshMSC GrowthMedium, andthen 1 � 105 MSCs were seeded on each ADM scaffold and continued to culture inthe MSC Growth Medium. For in vitro analysis, the scaffolds were cultured for up totwoweeks and the culture media were replaced every two days. For transplantationonto animal, these scaffolds were cultured for 1 day after seeded with MSCs.
2.4. Imaging instrument and methods
Nonlinear optical imaging, the TPF and SHG microscopic imaging was co-achieved in a two-photon system by using a commercial LSM 710 NLO confocalmicroscopy (Zeiss, Jane, Germany) equipped with a femtosecond Ti:Sapphire laser(Chameleon Vision Ⅱ, Coherent, Santa Clara, CA, USA), which provides a pulse lightwith tunable excitation wavelengths from 680 nm to 1080 nm. SHG imaging ofcollagen fiber was obtained by excitation at 820 nm, while GFP imaging of MSCs wasdone by excitation at 850 nm. The immunofluorescent images of CD-31, a-SMA andK10 were achieved in a single-photon system by using the commercial LSM 710 NLOconfocal microscopy (Zeiss, Jena, Germany) with the LASOS He/Ne gas laser operatedat 543 nm. The nuclei were imaged by excitation of DAPI either in two-photonsystem at 720 nm or single-photon system with the Coherent cube 405-FP solid-state laser operated at 405 nm depending on the convenience of non-transition ofimaging system in a same image frame. The laser light was in horizontal polarizationdirection and the optical signals were collected in the backward geometry.
2.5. Cell proliferation assay
In the co-cultured ADM scaffolds, MSC proliferation was quantitatively assessedby measuring the fluorescence intensity of GFP using ImageJ (NIH) software in 3Dmode [22]. After seeding onto the ADM scaffolds, most of the MSCs attached to theplates and ADM scaffolds after 6 h of incubation. On days 1, 4, 7, and 14, the ADMscaffolds were gently washed to remove non-adherent and dead cells and then fixedin 10% formalin prior to imaging. Images were taken by TPF and SHGmicroscopy andrecorded in 512 � 512 pixels with Plan-Apochromat 20X objectives (NA 0.8). Foreach sample (n ¼ 5 ADMs), 3 random fields were chosen within the ADM scaffoldand a stack of focal planes were taken from these 3 fields in the cellularized areausing a 5 mm step size. Fluorescent intensity of every field was analyzed using ImageJ(NIH) with the “3D object counter” plug-in. Each experiment was repeated threetimes. The proliferation indexes were based on the fluorescence intensity valuesexpressed relative to that of 14 day co-cultured ADM.
2.6. Wound model and ADM-MSC implantation
Eight-week-old BALB/c male mice were used. The dorsal skin of each mouse wasshaved and sterilized with 70% ethanol and iodine prior to surgery. Animals wereanesthetized with an intraperitoneal injection of chloral hydrate (400 mg/kg,Fuchen, Tianjin, China). Once the mice were anesthetized, a 7 mm biopsy punch wasused to make an impression on the dorsum, and then the circular region of tissuewas grabbed and pulled with forceps and excised with scissors to create a full-thickness wound. The wounded mice were divided into three groups, to betreated with ADM-MSC, ADM only or saline as control. After implanting ADM-MSC,ADM or saline, Comfeel transparent dressings (Coloplast, Beijing, China) were usedto cover the wound sites to prevent catching, biting and infection.
2.7. Histological and immunofluorescent analysis
Wound samples were harvested on designated days post-surgery. Samples werefixed in 10% formalin at room temperature for at least 24 h, embedded in paraffinand sectioned in 5 mm increments. Sections were made through the center of thewound and perpendicular to the skin surface. The sections were deparaffinized,rehydrated, washed in distilled H2O and stained with hematoxylin and eosin (H&E).For immunohistochemical staining, sections were placed in a citrate buffer(pH ¼ 6.0) and heated in a steamer for 10 min, and then blocked by incubation withPeroxide Block and normal goat serum (Beyotime, Shanghai, China). Samples werethen incubated overnight with primary antibodies against CD31, a-SMA and K10(1:1000, 1:1000, 1:200, respectively, Millipore Chemicon, Billerica, MA, USA) at 4
�C.
After washing, rhodamine-labeled secondary antibody (1:50, KPL, Gaithersburg,

Q. Wang et al. / Biomaterials 53 (2015) 659e668 661
MD, USA)was applied for 2 h. All sections were stained by DAPI (Sigma) for 15min tovisualize the nuclei. Sections were imaged by single-photon system and analyzed.Three random fields of each section (n ¼ 5) were chosen, and mature vessels con-taining erythrocytes were counted and measured using Image J (HIN) in order toevaluate the density and diameter of blood vessels in the wound areas.
2.8. Intravital imaging of ADM-MSC explants
After the mice were anesthetized and wound area sterilized (n ¼ 3), 5 randomregions were chosenwithin the wound area and were collected on days 1, 3, 5 and 7.These tissue samples were immersed in 0.9% SPSS (stroke-physiological saline so-lution) and then imaged by TPF and SHGmicroscopy using the stack scan mode. Theimaging system sequentially scanned the samples and a stack of focal planes weretaken along the z axis using a 2 mm step size. The consequent planes were thencomposed into a three-dimensional image on a computer screen. All procedureswere finished within 30 min to ensure that the chosen tissue samples were alive.
2.9. Skin maturity quantification
Skin structure was assessed on day 21 post-treatment using H&E-stained his-tologic sections, according to previously published methods [23,24]. Specific criteriawere used to assess each wound for dermal differentiation, epithelial maturation,and skin appendage regeneration.
I. Dermal differentiation grading was defined based on following 4-grade criteria:1, thin, dense, and monotonous fibrosis;2, thicker but still dense and monotonous fibrosis;3, two layers but not completely discreet;4, two discreet layers with superficial fibrosis and loose alveolar tissue withinthe deep layer;
II. Epithelial maturation grading used the following criteria:1, thin and with no reticulation;2, occasional reticulation;3, moderate reticulation;4, thick with complex reticulation;
III. Skin appendage regeneration grading was defined according to the followingcriteria:1, no developing glandular structure;2, minimal developing glandular structure;3, considerable developing glandular structure;4, mature glandular structure and developing hair follicles.
2.10. Statistical analysis
All data are represented as means ± standard deviation (SD) with at least threeindependent replicates. Difference between groups was analyzed by two-tailedStudent's t-test. A p value <0.05 was considered to be statistically significant.
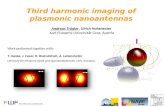
Fig. 1. Characterization of ADM scaffolds. (A) The appearance of ADM after decellularizatioreveals the absence of cell components in ADM. (C) SHG imaging of ADM in vitro proviorientation, and structure characteristics of collagen fibers in ADM. (Bottom) Papillary dermphotograph displays a huge cavity in the scaffold caused by removal of hair follicles via thesubtle structure of collagen fibers at high magnification. Scale bar, 100 mm (B and C), 10 mm
3. Results
3.1. Characterization of mouse ADM
The average thickness of ADMs after the treatment of deep-ithelization and decellularization was measured to be0.58 ± 0.17 mm (n ¼ 5). SHG microscopy and SEM images revealedthe shape, orientation, density of collagen fibers and the spaciousstructure characteristics of ADM scaffolds. DAPI-staining nucleiwere not found in ADM sections (Fig. 1).
3.2. Proliferation of MSCs on ADM scaffolds in vitro
Fig. 2A and B shows the different morphological characteristicsof MSCs grown on different surfaces. MSCs grown on ADM had amore elongated and spindle-like shape (Fig. 2B) than those culturedin a dish (Fig. 2A); this may have been caused by the rough surfaceof the ADM. These EGFP-labeled MSCs exhibited bright greenfluorescence under the fluorescent microscope (Fig. 2A and B).
The proliferation of MSCs in scaffolds was monitored using two-photon system. The distribution and amount of MSCs weremeasured on different co-culture days after these MSC-seededscaffolds were fixed and stained directly with DAPI. MSCscontinued to proliferate in the scaffolds and MSCs graduallyinvaded deeper layers of scaffolds. In Fig. 2C, the MSC nuclei indeeper layers appeared out of focus (white arrows) compared tothose on the surface of ADM. To determine the spreading distance,the ADM-MSC scaffolds (n ¼ 5) were scanned for GFP fluorescencein 0.5 mm steps, and the depth from the surface to the first plane inwhich fluorescence from MSCs disappeared was defined as thedistance of cell spreading. On days 1, 7 and 14, these distancesreached 4.61 ± 1.27 mm, 15.94 ± 3.18 mm, and 32.06 ± 2.30 mmrespectively (Fig. 2E). Fig. 2D and F shows the MSC proliferation inADM scaffolds on days 1, 4, 7 and 14, with proliferation indexes of0.18 ± 0.07%, 0.32 ± 0.04%, 0.45 ± 0.11% and 100 ± 0.09%,respectively. The proliferation indexes were based on the fluores-cence intensity values expressed relative to that of 14 day co-cultured ADM.
n treatment in a 30 mm culture dish. (B) Imaging of ADM section with DAPI-stainingdes a new means to visualize collagen fibers. (D) SEM images of ADM show shape,is side photograph shows arrangement of collagen fibers in ADM; (Top) Epidermis sidedecellularization process; (Fibers) Papillary dermis side photograph exhibits the more(D-Bottom and D-Top), 1 mm (D-Fibers).

Q. Wang et al. / Biomaterials 53 (2015) 659e668662
3.3. MSC-ADM promotes wound healing in vivo
Mice were euthanized on days 7, 14 and 21 post-treatment, forclinical observation and histological analysis. The wound healingprocess was significantly accelerated in the ADM-MSC and ADMgroups compared with the control group (Fig. 3A and B). In thecontrol group, even on day 21, thewoundswere still not fully closedand were covered with eschar in some areas. In addition, the re-generated skin in the control group was translucent and thin, withno skin appendage regeneration. In ADM group, the borders be-tween grafts and wounds were distinguishable and skin appendagehad started to regenerate in forming skin. In the ADM-MSC group,the peripheral region of the wound appeared to have integratedinto the surrounding native skin tissue and there was completeappendage regeneration.
Collagen structures in the dermis of regenerated skin in threegroups at day 21 were visualized by combined TPF/SHG imaging.Fig. 3C shows that the underlying network structure of collagenfibers in ADM-MSC group was well organized and morphologicallycloser to normal dermal tissue. The collagen content was lower andfibers more scattered in the ADM and control groups 21 days after
Fig. 2. Spreading and proliferation of MSCs in vitro. (A) and (B) The fluorescent imaging ofseeded on ADM displayed a more elongated shape than those cultured in the dish. (C) TPcultured for 4 days in MSC Culture Medium prior to imaging. Some MSCs have entered into a4, 7 and 14, respectively. (E) Measurement of the invasion depth of MSCs in the ADM on daydays 1, 4, 7 and 14 by estimating the fluorescent intensities from the images with ImageJ (loaded on the ADM scaffold. Scale bar, 100 mm (A, B and D), 20 mm (C).
surgery indicating that the healing dynamics were accelerated inthe ADM-MSC group compared to the ADM and control groups.
3.4. Evaluation of angiogenesis response
The angiogenic response, an important step in healing process forsevere injuries, was also analyzed. Immunohistological staining ofwound sections was done for the endothelial protein CD31 (Fig. 4A).Early vascular networks and a large number of endothelial cells werepresent in and around thewounds treated with ADM-MSC, but werenot observed in wounds treated with only ADM or saline.
Alpha-smooth muscle actin (a-SMA) staining of wound sectionsof different treatments on day 14 identified vasculature stabilizedwith smooth muscle cells. A significant increase in vascular net-works layered with smooth muscle cells was also seen within thewounds treated with ADM-MSC (Fig. 4B). There was only a smallamount of vascular vessels and smooth muscle cells found inwounds treated with ADM or saline. Blood vessel density wassignificantly higher in wounds treated with ADM-MSC (337 ± 50/mm2) vs. wounds treated with ADM (121 ± 24/mm2) or saline only(49 ± 24/mm2). Moreover, vessel diameter was larger in the healing
MSCs (GFP-tagged) cultured in a Petri dish and co-cultured with ADM. On day 1, MSCsF/SHG image of ADM-MSC scaffold surface. In this photograph, the scaffold has beendeep layer of ADM (white arrows). (D) Images of MSC proliferation on ADM on days 1,
s 1, 7 and 14, respectively. (F) Quantitative analysis of MSC proliferation on the ADM onNIH) software. Values are relative to that of the MSCs cultured for 14 days after being

Q. Wang et al. / Biomaterials 53 (2015) 659e668 663
tissues of the ADM-MSC group comparedwith the ADM and controlgroups (24.54 ± 7.21 mm,15.54 ± 2.13 mm, 8.79 ± 1.64 mm) (Fig. 4D).These data indicate that ADM-MSC promoted the recruitment ofendothelial cells to the wound area and enhanced vessel growth inhealing wounds.
3.5. Evaluation of skin re-epithelialization
Sections of the wounds were stained with the epithelial proteincytokeratin 10 (K-10) to evaluate re-epithelialization. Layeredepithelial structures were observed in wound areas of mice in theADM-MSC group at 14 days post-surgery, however these were notobserved in the ADM group mice. In the control group mice, thewounds were still covered with eschar (Fig. 5A, C and E). Maturedepithelial structures were observed in mice in the ADM-MSC group21 days post-surgery. In contrast, the epithelial layers of ADM andcontrol group mice were thinner and the K-10 positive cells wereobserved in random positions (Fig. 5B, D, and F). These resultssuggest that ADM-MSC contributed to re-epithelialization andappendage regeneration of skin wounds.
3.6. Intravital imaging of ADM-MSC graft
The activity of MSCs seeded in ADM grafts and the collagen inregenerated tissue in the wound environment were analyzedwithin 1 week in order to further investigate the impact of ADM-MSC in skin wound healing. The imaging process was conductedas outlined in Fig. 6A. Intravital imaging of the ADM-MSC grafts(Fig. 6B) revealed that the MSCs seeded in the ADM migrated from
Fig. 3. Effects of ADM-MSC treatment on wound healing. (A) Macroscopic observation of msentative photographs of the wounds on days 7, 14 and 21 (after removal of Confeel dressingMSC promoted wound healing with less eschar and skin appendage regeneration. (C) TPstructures had formed in dermal layer at 21 days after treatment. Nuclei were stained with D0.6 cm (A), 100 mm (B), 50 mm (C).
the scaffolds (the layer at a depth 120 mm) to the regenerated tissuein the bottom (the layer at a depth 20 mm). The numbers of liveMSCs within different areas were determined by GFP fluorescenceintensity. As shown in Fig. 6C, the number of cells graduallydecreased in the 120 mm layer and no cells were observed after 5days. In the 20 mm layer, the cell number increased. The cell numberin the middle and border areas was also analyzed at 5 and 7 days.The numbers of cells in these two areas were approximately thesame on day 5 (Fig. 6D). However, on day 7 there were more cells inthe border areas than in the middle areas. The results above indi-cate that, after being grafted to the wounds, the MSCs moved to theregenerated tissue from the ADM-MSC scaffolds and they survivedin the regenerated tissue for at least one week, especially in theperiphery of lesions.
On day 1 after the treatment, degradation of ADM scaffolds(120 mm layer) was observed in both the ADM-MSC and ADMgroups compared to an ungrafted ADM scaffold (Fig. 6E). Also, thedegradation of collagen fibers was more significant in the ADM-MSC group than in the ADM group. By day 3, the scaffolds in theADM group tended to be degraded more than on day 1 and theADM scaffolds were hardly detectable in the ADM-MSC group.
As shown in Fig. 6F and 1 day after grafting in the ADM-MSCgroup, the collagen network appeared in the regeneration bottomlayer and was only detected in the ADM group 5 days after treat-ment (Data was not shown). On day 7, the regenerated collagennetwork was close to that in normal skin tissue in morphology.Fig. 6E revealed that the regeneration of collagen networksoccurred earlier and more completely in the ADM-MSC groupcompared to the ADM group.
urine skin wounds after treatment with ADM-MSC, ADM, or saline (control). Repre-). (B) Representative images of HE-stained histological wound sites, showing that ADM-F/SHG images of the regenerated skin in the 3 groups showed that distinct collagenAPI. W, wound site; A, ADM scaffold; E, eschar; S, sebaceous gland; F, follicle. Scale bars,

Q. Wang et al. / Biomaterials 53 (2015) 659e668664
3.7. Evaluation of skin regeneration
Regenerated skin structure was analyzed by dermal differenti-ation, epithelial maturation and skin appendage regeneration(n¼ 10). The scores of these groups imply that ADM-MSC promotedsignificant skin maturation. The ADM-MSC wounds had defineddermal structures and mature epithelial structures with sebaceousglands and hair follicles. As shown in Fig. 7A, the histological scoresof the ADM-MSC group at 21 days were significantly higher thanboth the ADM and the control groups (p < 0.05). Furthermore,when the treatment was extended to 35 days, ADM-MSC promotedcomplete skin regeneration and integration into normal skin, withno wound contraction. However, visible scars and contraction oflesions were found in both ADM and control groups at 35 days andthe regenerated skin was thin and frail in the control group(Fig. 7B).
4. Discussion
Various strategies, such as epidermal replacement, engineereddermal constructs and engineered skin substitutes, have been
Fig. 4. Effects of ADM-MSC on Angiogenesis. (A) Endothelial cell infiltration. Immunofluoredotted line represents the interface between regenerated tissue and implanted scaffold. (B) Aof vessel density and vessel diameter in wound sites of 3 groups based on SMA staining. Thestained with DAPI. R, regenerated tissue; S, implanted scaffold; Scale bar, 50 mm. Values sh
developed to use as skin replacements for wound management[25]. ADM is a dermal substitute that retains the native structure ofdermis. Complete removal of cellular components reduces theimmunogenicity of allogeneic and xenogeneic biologic scaffolds,and may facilitate tissue remodeling [26]. Alternatively, MSCs havebeen an attractive cell source for regenerative medicine for treat-ment of skin injuries. Successfully using MSCs for skin regenerationrequires a sufficient quantity of MSCs and effective delivery of theMSCs to the wound site. Theoretically, ADM can serve as a scaffoldfor the delivery of MSCs to the target wound, while the MSCspromote retention and neovascularization of the scaffold [27].
In this study, we demonstrated that MSCs could attach in vitro toADM prepared from male BALB/c mice. Previous research hasestablished that burns exhibit minimal scar formation if they areprimarily healed in less than 21 days whereas, if healing isincomplete at 21 days, satisfactory regeneration is unlikely [28]. Inthe current study, at 21 days after treatment, wound closure and re-epithelialization were enhanced and vascular density around thewounds were higher in the ADM-MSC group compared with theADM and control groups. Furthermore, full-thickness excisionalwounds were improved and repaired with allogeneic ADM graft
scence of wound sections of 3 groups on day 7 after treatment, stained for CD31. Thengiogenic response of SMA staining on day 14 of treatment. (C) and (D) Quantificationresults showed that ADM-MSC promoted angiogenesis in wound sections. Nuclei wereown are means ± SD. *p < 0.05, **p < 0.01.

Fig. 5. Effects of ADM-MSC on re-epithelialization. In control, ADM and ADM-MSC groups, confocal observation of wound sections, immunostained with K-10, are shown on day 7(A, C and E) and day 14 (B, D and F) after treatment. These results revealed that ADM-MSC contributed to re-epithelialization. Nuclei were stained with DAPI. Scale bar, 50 mm.
Q. Wang et al. / Biomaterials 53 (2015) 659e668 665
treatment and the improvement and repair was even more sig-nificant, and included complete skin appendage regeneration,when wounds were treated with MSC-seeded ADM grafts. Anotherconsideration for wound repair is the formation of scars, which arecaused by deposition of excess ECM by fibroblasts in the woundbed. These structures carry a variety of undesirable consequences,including unsightly appearance on the skin. In addition, scars lackmuch of the normal makeup of the skin, such as follicles and nerveendings and also do not retain the normal tensile strength of un-damaged skin [29]. Excess ECM synthesis by fibroblasts is caused byinsufficient dermal components in the wound bed. The utilizationof ADM scaffolds can provide a sufficient amount of dermal tissueto reduce scar formation and contraction in wound healing. MSC-based cell therapy, in combination with matrix scaffolds, hasbecome a potential strategy used in many clinical treatments toimprove wound healing outcomes [30]. A similar study was doneby Anlun M. et al., in which the transplantation of an ADM-MSCscaffold contributed to the healing process of cartilage defects ina monkey model [31].
Fig. 6. The activity of MSCs and ECM in the wound sections. (A) Diagram of the intravital imagraft was implanted. (b) Random wound areas were chosen and collected in border and miscaffold layer along the z axis. (B) TPF/SHG 3D scanning images of living wound tissue harvesnumbers on a 20 mm layer and a 120 mm layer of each selected section based on (B). Valuetreatment. (D) The percentages of MSCs in middle and border areas at 5 and 7 days. (E) Dtreatment. (F) Regeneration of the collagen network in newly formed tissue. The results prothe ADM-MSC scaffolds. The degradation and regeneration of the ECM around the junction aGreen-GFP of MSCs. Scale bar, 100 mm (E), 50 mm (F). Values expressed as means ± SD.
Revascularization of the wound bed is a crucial stage during thenormal wound healing process. New vessels form and develop inthe granulation tissue to supply oxygen and nutrients to the woundarea. Angiogenesis is a complex process that is controlled by thebalance of proangiogenic and antiangiogenic factors [32]. MSCsplay an important role in this process and endogenous MSCs aremobilized and recruited to the wound bed [33]. In the currentstudy, both the exogenous MSCs and endogenous endothelial cellswere recruited to the regenerated tissue in the ADM-MSC group at7 days post-treatment. Also, the density of stable and functionalvessels was higher in the newly formed dermal layers in ADM-MSC-treated wounds after 14 days, suggesting that exogenousMSCs can promote angiogenesis. Relative studies have demon-strated that mesenchymal cell type is necessary to establish amature vascular network either in vitro [34] or in vivo [35]. Otherresearch has suggested that the improved MSC-mediated angio-genesis is partially related to the release of proangiogenic factors[36], such as VEGF-a and Ang-1, which play key roles in angio-genesis by stimulating endothelial cell proliferation, migration, and
ging procedure of ADM-MSC grafts. (a) The wound model was made and the ADM-MSCddle areas. (c) Tissue samples were scanned from the regenerated bottom layer to theted from ADM-MSC groups, 1, 3, 5, and 7 days after treatment. (C) Quantification of cells are relative to the fluorescent intensities of the MSCs on 20 mm layer after 7 days ofegradation of ADM scaffolds in the junction areas in 2 groups on days 1 and 3 afterved that, after implantation, the MSCs tended to move to the newly formed tissue fromrea occurred earlier in ADM-MSC group compared to ADM group. Red-SHG of collagen,

Fig. 6. (continued).
Q. Wang et al. / Biomaterials 53 (2015) 659e668666
organization into tubules. In our model, further experiments areneeded to determine whether the exogenous MSCs promotedangiogenesis by secreting these proangiogenic factors or bydifferentiating into pericytes to facilitate vessel maturation.
Dermal tissue undergoes dynamic changes during woundhealing. These changes have been extensively investigated viahistological methods in fixed skin biopsy specimens. However, suchex vivo assessment methods have often limited utility since only

Fig. 7. Evaluation of regenerated skin tissue. (A) Histological analysis scores of woundsin terms of dermal differentiation and epithelial and skin appendage regenerationaccording to the description in the Materials section. The histological scores of theADM-MSC group were much higher at 21 days. (B) Photos of wound healing in the 3groups, 5 weeks after grafting treatment, indicated that ADM-MSC contributed tocomplete skin regeneration. Values shown are means ± SD. *p < 0.05, **p < 0.01.
Q. Wang et al. / Biomaterials 53 (2015) 659e668 667
thin tissue slices stained with extrinsic dyes can be analyzed. Thedevelopment of methods that detect intrinsic signals in minimallyprocessed tissues will greatly improve our understanding of theskin conditions and diseases [37,38]. Recently, the collagen-sensitive SHG microscopic imaging technique has been widelyused for ECM imaging in the biomedicine field, even for the in vivoassessment of collagen structure changes during human skin aging[39,40]. This method provides unique imaging characteristics, suchas high image contrast, high spatial resolution, optical 3Dsectioning, minimal invasiveness, deep penetration and no inter-ference from background light. Most importantly, the tissue can beclearly visualized without additional staining. In the current study,the combined TPF/SHG imaging technique was used for the firsttime as a complement to traditional methods for assessing the skinwound healing process. The 3D images (Video. 1) clearly revealedthe activity of seededMSCs inwound tissue as well as the dynamicsof dermal collagen network around MSCs in different scanninglayers. Our results demonstrated that the MSCs migrated towardsand survived in the newly formed bottom layer. Post-implantationcell survival is critical for the successful use of MSCs in any potentialcell therapy, since it eliminates the need to repeatedly inject thesecells. Moreover, the collagen fibers within the ADM scaffoldsdegraded sooner in the ADM-MSC group than in the ADM group.The regeneration of the collagen network also occurred earlier (1day after treatment) in the ADM-MSC group than in the ADM-onlygroup (5 days after treatment). In skin wounds, the deposition ofECM is an essential step for cell adhesion, cell proliferation andintegration of the cell/biomaterial hybrid into the surroundingtissue. The degradation of ADM scaffold might be induced by the
seeded MSCs, although further experiments are needed to confirmthis connection.
Supplementary video related to this article can be found athttp://dx.doi.org/10.1016/j.biomaterials.2015.03.011.
5. Conclusion
In conclusion, the current study clearly demonstrated that MSC-seeded ADM scaffolds promoted significant neovascularization,ECM remodeling and complete skin regeneration and have greatpotential as a unique device for superior clinical treatment of full-thickness skin wounds. Furthermore, the nonlinear optical imag-ing technique used in this study provided an additional method forassessment of wound healing.
Acknowledgments
This work was supported by the National Natural ScienceFoundation of China (No.81171379) and Instrument functionaldevelopment and technological innovation projects of CAS(No.yg2012048).
References
[1] Gurtner GC, Werner S, Barrandon Y, Longaker MT. Wound repair and regen-eration. Nature 2008;453:314e21.
[2] Zhang XJ, Deng ZH, Wang HL, Yang ZH, Guo WH, Li Y, et al. Expansion anddelivery of human fibroblasts on micronized acellular dermal matrix for skinregeneration. Biomaterials 2009;30(14):2666e74.
[3] Feng Y, Wang J, Ling S, Li Z, Li M, Li Q, et al. Differentiation of mesenchymalstem cells into neuronal cells on fetal bovine acellular dermal matrix as atissue engineered nerve scaffold. NRR 2014;9:1968e78.
[4] Rennert RC, Sorkin M, Garg RK, Januszyk M, Gurtner GC. Cellular response to anovel fetal acellular collagen matrix: implications for tissue regeneration. Int JPolym Mater 2013;2013:527957.
[5] LdS Meirelles, Caplan AI, Nardi NB. In search of the in vivo identity ofmesenchymal stem cells. Stem Cells 2008;26:2287e99.
[6] Sharma RI, Snedeker JG. Paracrine interactions between mesenchymal stemcells affect substrate driven differentiation toward tendon and bone pheno-types. PloS One 2012;7:e31504.
[7] Vishnubalaji R, Al-Nbaheen M, Kadalmani B, Aldahmash A, Ramesh T. Skin-derived multipotent stromal cells - an archrival for mesenchymal stem cells.Cell Tissue Res 2012;350:1e12.
[8] Crisan M, Yap S, Casteilla L, Chen C-W, Corselli M, Park TS, et al. A perivascularorigin for mesenchymal stem cells in multiple human organs. Cell Stem Cell2008;3:301e13.
[9] Caplan A. Why are MSCs therapeutic? New data: new insight. J Pathol2009;217:318e24.
[10] Caplan AI. All MSCs are pericytes? Cell Stem Cell 2008;3:229e30.[11] Schneider RK, Puellen A, Kramann R, Raupach K, Bornemann J, Knuechel R,
et al. The osteogenic differentiation of adult bone marrow and perinatalumbilical mesenchymal stem cells and matrix remodelling in three-dimensional collagen scaffolds. Biomaterials 2010;31:467e80.
[12] Schneider RK, Püllen A, Kramann R, Bornemann J, Knüchel R, Neuss S, et al.Long-term survival and characterisation of human umbilical cord-derivedmesenchymal stem cells on dermal equivalents. Differentiation 2010;79:182e93.
[13] Schneider RKM, Neuss S, Stainforth R, Laddach N, Bovi M, Knuechel R, et al.Three-dimensional epidermis-like growth of human mesenchymal stem cellson dermal equivalents: contribution to tissue organization by adaptation ofmyofibroblastic phenotype and function. Differentiation 2008;76:156e67.
[14] Nie C, Yang D, Morris SF. Local delivery of adipose-derived stem cells viaacellular dermal matrix as a scaffold: a new promising strategy to acceleratewound healing. Med Hypotheses 2009;72:679e82.
[15] Campagnola PJ, Clark HA, Mohler WA, Lewis A, Loew LM. Second-harmonicimaging microscopy of living cells. J Biomed Opt 2001;6:277e86.
[16] Helmchen F, Denk W. Deep tissue two-photon microscopy. Nat Methods2005;2:932e40.
[17] Campagnola PJ, Millard AC, Terasaki M, Hoppe PE, Malone CJ, Mohler WA.Three-dimensional high-resolution second-harmonic generation imaging ofendogenous structural proteins in biological tissues. Biophys J 2002;82:493e508.
[18] Zoumi A, Yeh A, Tromberg BJ. Imaging cells and extracellular matrix in vivo byusing second-harmonic generation and two-photon excited fluorescence.PNAS 2002;99:11014e9.

Q. Wang et al. / Biomaterials 53 (2015) 659e668668
[19] Freund I, Deutsch M, Sprecher A. Connective tissue polarity. Optical second-harmonic microscopy, crossed-beam summation, and small-angle scatteringin rat-tail tendon. Biophys J 1986;50:693e712.
[20] Campagnola PJ, Loew LM. Second-harmonic imaging microscopy for visual-izing biomolecular arrays in cells, tissues and organisms. Nat Biotechnol2003;21:1356e60.
[21] Zipfel WR, Williams RM, Webb WW. Nonlinear magic: multiphoton micro-scopy in the biosciences. Nat Biotechnol 2003;21:1369e77.
[22] Mathieu E, Lamirault G, Toquet C, Lhommet P, Rederstorff E, Sourice S, et al.Intramyocardial delivery of mesenchymal stem cell-seeded hydrogel pre-serves cardiac function and attenuates ventricular remodeling after myocar-dial infarction. PLoS One 2012;7:e51991.
[23] Ehrbar M, Djonov VG, Schnell C, Tschanz SA, Martiny-Baron G, Schenk U, et al.Cell-demanded liberation of VEGF(121) from fibrin implants induces local andcontrolled blood vessel growth. Circ Res 2004;94:1124e32.
[24] Sun G, Zhang X, Shen Y-I, Sebastian R, Dickinson LE, Fox-Talbot K, et al.Dextran hydrogel scaffolds enhance angiogenic responses and promotecomplete skin regeneration during burn wound healing. PNAS 2011;108:20976e81.
[25] Clark RAF, Ghosh K, Tonnesen MG. Tissue engineering for cutaneous wounds.J Invest Dermatol 2007;127:1018e29.
[26] Portmann-Lanz CB, Ochsenbein-Koelble N, Marquardt K, Luethi U, Zisch A,Zimmermann R. Manufacture of a cell-free amnion matrix scaffold that sup-ports amnion cell outgrowth in vitro. Placenta 2007;28:6e13.
[27] Huang S-P, Hsu C-C, Chang S-C, Wang C-H, Deng S-C, Dai N-T, et al. Adipose-derived stem cells seeded on acellular dermal matrix grafts enhance woundhealing in a murine model of a full-thickness defect. Ann Plas Surg 2012;69:656e62.
[28] Cubison TCS, Pape SA, Parkhouse N. Evidence for the link between healingtime and the development of hypertrophic scars (HTS) in paediatric burns dueto scald. Burns 2006;32:992e9.
[29] Singer AJ, Clark RAF. Mechanisms of disease - cutaneous wound healing. NewEngl J Med 1999;341:738e46.
[30] Maxson S, Lopez EA, Yoo D, Danilkovitch-Miagkova A, Leroux MA. Concisereview: role of mesenchymal stem cells in wound repair. Stem Cells TranslMed 2012;1:142e9.
[31] Ma A, Jiang L, Song L, Hu Y, Dun H, Daloze P, et al. Reconstruction of cartilagewith clonal mesenchymal stem cell-acellular dermal matrix in cartilage defectmodel in nonhuman primates. Int Immunopharmacol 2013;16:399e408.
[32] Arnold F, West DC. Angiogenesis in wound healing. Pharmacol Ther 1991;52:407e22.
[33] Chun JL, O'Brien R, Song MH, Wondrasch BF, Berry SE. Injection of vessel-derived stem cells prevents dilated cardiomyopathy and promotes angio-genesis and endogenous cardiac stem cell proliferation in mdx/utrn-/- but notaged mdx mouse models for duchenne muscular dystrophy. Stem Cells TranslMed 2013;2:68e80.
[34] Boyd NL, Nunes SS, Krishnan L, Jokinen JD, Ramakrishnan VM, Bugg AR, et al.Dissecting the role of human embryonic stem cell-derived mesenchymal cellsin human umbilical vein endothelial cell network stabilization in three-dimensional environments. Tissue Eng Part A 2013;19:211e23.
[35] Koike N, Fukumura D, Gralla O, Au P, Schechner JS, Jain RK. Creation of long-lasting blood vessels. Nature 2004;428:138e9.
[36] Wu Y, Chen L, Scott PG, Tredget EE. Mesenchymal stem cells enhance woundhealing through differentiation and angiogenesis. Stem Cells 2007;25:2648e59.
[37] Konig K, Riemann I. High-resolution multiphoton tomography of human skinwith subcellular spatial resolution and picosecond time resolution. J BiomedOpt 2003;8:432e9.
[38] Palero JA, de Bruijn HS, van der Ploeg-van den Heuvel A, Sterenborg H,Gerritsen HC. In vivo nonlinear spectral imaging in mouse skin. Opt Express2006;14:4395e402.
[39] Koehler MJ, Koenig K, Elsner P, Bueckle R, Kaatz M. In vivo assessment ofhuman skin aging by multiphoton laser scanning tomography. Opt Lett2006;31:2879e81.
[40] Masters BR, So PTC. Confocal microscopy and multi-photon excitation mi-croscopy of human skin in vivo. Opt Express 2001;8:2e10.